August 7
3 AM
My gallbladder (an issue that I’ve been struggling with since about 27 weeks) decided to get the party started at 3 AM. By about 9 that evening, I was in the midst of one of my worst flare ups, and opted to call the on-call midwife at my clinic to see if I should wait things out or head in to the ER for monitoring. My pain was pretty unbearable, and I was worried about a full on blockage/rupture. She recommended that I head in, at least for pain management since Tylenol and heat packs at home weren’t cutting it. She called ahead to the birthing center and had them set up a bed for me so I wouldn’t have to wait in the ER. (SO ETERNALLY GRATEFUL FOR THAT)
10:30 PM
We grabbed our go-bags (just in case) and checked in. They sent me to triage and the nurse hooked me up to some monitors while we waited. She went to call the midwife about offering some heavier medication and ask about a plan. About 20 minutes in, baby’s heart rate went really high (like 200), and then dropped down to 30bpm for almost a full minute. Suddenly the room filled with nurses, I was turned on my side and they started looking for veins for an IV. Baby’s heart rate stabilized, but they opted to start me on some fluids and IV pain meds just to be safe.
Soon the midwife I had chatted with came in and said she was recommending an ultrasound to check the gallbladder, and then to admit me overnight to keep an eye on Baby after the dip on the monitor. We agreed and soon moved into a room for the night.
AUGUST 8
6AM
The next morning, the midwife came in to let me know she’d been talking with the general surgeon and the GI specialist about how we should proceed, and both recommended (after my ultrasound) that we move towards induction so we can start looking towards gallbladder removal.
Since they were full for Saturday inductions, she put me on the schedule for Sunday night. Since Baby had been stable all night, my pain was adequately controlled, and I was able to eat without another flare, she felt comfortable sending us home to rest, prepare, eat our own food, and get ready to meet our baby.
10 AM
Discharged and on our way home, with anticipation filling our guts. We couldn’t believe we went from zero to a hundred so quickly, but we were so excited to know the end was in sight and Baby would be here soon. At this point I felt really lucky to be at home, knowing it was one of our last nights together. We had a “date night” at home and watched movies and relaxed. I took a long bath, painted my toes, and enjoyed what would be my last full nights rest for some time. (I was amazingly able to get 9+ hours!)
August 9
We spent most of this day cleaning and getting all our last minutes needs taken care of. I set up breastfeeding stations, and gathered the last of what I needed for my hospital bag. Kyle cleaned the house top to bottom and got everything he needed packed and ready.
6:30 PM
We check in to labor and delivery and get set up in our room. The midwife came in and reviewed that we would be starting on Misoprostel to help ripen what was currently a very closed and posterior cervix (my check with the first midwife the day before confirmed I wasn’t dilated at all.) She told us it was an oral medication that I could take up to 6 times in 12-24 hours depending on how it goes.
I was hooked up to monitors again, given an IV and my first dose of meds before they turned out our lights and told us to get some sleep.
11PM(ish)
The Misoprostel started regulating a few of my contractions, which I could feel but weren’t painful. The tightening made it hard to sleep, as did the nurses coming in to adjust the baby’s monitor. Baby kept jumping off the monitors, so they would come in and slide the sensor around until they found it.
August 10
6 AM
The overnight midwife came in and asked if she could check my cervix to see where things were at. I was hopeful that the regular contractions I had felt most of the night had been progress, but was very discouraged to hear (after an incredibly painful exam) that I was only dilated to a 1.5 and still very posterior. I was in tears after the exam, and honestly felt a little traumatized. She recommended that we try a “cooks catheter” and felt confident she could get it in, despite how high everything still was. Desperate to make more progress I agreed. And let her place it. Again—it was incredibly painful and tense.
(For those of you who don’t know a cooks catheter is a manual ripening agent rather than medication based. It has two balloon parts one that sits inside the cervix, and one right below) the balloons are filled with saline, and the weight of them essentially pulls and puts pressure on the cervix to open and dilate. Sounds fun huh?)
After placement, I had what ended up being the most excruciating part of my labor experience. They had warned my I might feel “a little crampy,” but what I ended up feeling was each contraction practically ripping my pelvis into shreds. I was lying in bed, unable to sit up, bawling through each wave of pain, holding Kyle’s hand. This went on for about 2 hours. I told him through tears that I couldn’t do it anymore and that I would definitely be needing an epidural if I had to have this kind of pain for the next 12-24 hours.
8 AM
I was relieved to hear my regular midwife was now the on call midwife, and seeing her face was so SO good. She was the one I’d seen for all my prenatal appointments, and she knew me and what my plan for labor had been. She came in to touch base and for the first time someone actually asked me how I was doing, not just physically but mentally and emotionally. I cried through my explanation of how I was feeling, and finally felt comfortable asking about some of the what if’s ahead of us. She shared in my desire for a natural labor and confirmed that the few hours after catheter placement were the worst and I should have relief soon. She did tell me that I was not uncommon for induced mamas to need an epidural, and while she would help us do everything we could to stay on goal, she helped me come to terms with the fact that there was absolutely no shame in asking for the extra medication.
The rest of the day was spent trying to stay as comfortable as possible. In the evening, my midwife offered to start me on low dose pitocin to help the catheter do its job a little faster. While I was nervous about starting it, and having more painful contractions, I agreed. We were pretty desperate to make some progress at this point.
My regular midwife, who had been checking on me regularly, let us know that she was pretty sure she wouldn't be around to deliver the baby, but she told us about the next on call midwife and assured us that she would be wonderful and we would like her a lot.
August 11
Around 1 AM they came in to pull the catheter. Unfortunately I wasn’t dilated enough for it to fall out on it’s own, but the nurse didn’t have to fully deflate it to get it out, so we were hopeful. This next check confirmed I was at a 4.5-5cm and I was SO relieved that we had made progress. Because it was still considered a “manual” dilation, we opted to try the third and final method of ripening, Cervidil. This is a medication they place inside the cervix, and placement was so much easier than the catheter. (THANK GOD) I was taken off the Pitocin drip, but kept baby monitors on.
I was finally able to get some rest and slept from 2-6AM. I got up to use the restroom that morning, and the Cervidil they placed fell out. I had Kyle page the nurse, and she did another check—where she happily reported I was at a 6!
I was able to eat breakfast (first meal in almost 24 hours) and take a shower, and then the new midwife came on and we got started on Pitocin—but for real this time, no more low dose.
We were hopeful that this meant baby would come soon! I made a joke about how grateful we were that despite my gallbladder being the reason we were admitted—it had stayed dormant this whole time.
Around lunch time, I started to feel my the familiar pain—my gallbladder decided to make me a liar. At first I wasn’t concerned, but then it started to pick up and before I knew it, I was doubled over in pain.
My wonderful nurse came in and offered a heat pack, Tylenol, and then finally some Fentanyl. That first does of Fentanyl hit me with a beautiful wave of relief, and laying on the heat pack helped me relax into a nap.
I took a few more doses of fentanyl over the course of the afternoon, but it unfortunately is less effective with each dose, and the last one only lasted about 10 minutes.
At this point I was seriously considering the epidural route simply because I knew I would not be able to cope with a gallbladder flare and any painful contractions.
I had them send the anesthesiologist in to talk about placing it a little higher in order to touch my gallbladder. He unfortunately said they wouldn’t dose it that high for labor, due to the expanded list of risks associated with higher dosing.
After discussing it, Kyle and I both agreed that the epidural route was going to be the best way for us to go--I was exhausted, and still in a lot of pain from my gallbladder.
Our daytime nurse (who I really liked) rounded us onto the overnight crew and we met Zoey--the nurse who changed my life and honestly carried us all through the delivery. She was spunky, and knowledgeable, and we LOVED her. It was around this time that I asked for the epidural--and she started me on the fluids I would need beforehand. My contractions were well regulated with the Pitocin, but I wasn't feeling them very much.
7pm (Ish)
Zoey helped get me comfortable, and then told us to try and get some rest. I started feeling the pressure from my contractions very regularly, and she told me to page her if I started to feel like I needed to poop.
August 12
12 AM
I was lying on my right side, straddling the peanut ball, trying to nap (lol) and I started to feel each contraction in my left hip--almost like a hotspot. It was definitely more than "pressure," but it wasn't excruciating. I asked Zoey to help me turn when she came in to check on me, and told her about he pain. She recommended that I try adding an extra dose of meds from the epidural, and turn on my other side to let gravity do it's job with spreading the medication. I did two extra doses before I felt any relief, but it was welcome when it came. I mentioned to Zoey that I could feel consistent pressure in my pelvis through each contraction, but that it subsided when the contractions subsided--it wasn't constant like she had mentioned it might be. She decided to call the midwife down just in case, and started getting things in the room pulled out. She also paged "the baby nurse" to come get set up. It started to feel like it was time, but I was trying not to get too excited. I knew that after they broke my water we were on a time crunch but after three days, I felt like the baby was never coming out.
1:30 AM
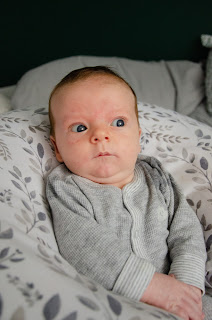
It honestly felt like no time at all--which compared to everything else it wasn't, but an hour after I started pushing, baby popped out, and Kyle got to tell me that it was a BOY!
I still can't really grasp or describe how surreal it was to go from being pregnant to having a baby placed on my chest, and having him here. We spent the next hour with him on my chest, getting him latched to start breastfeeding, and cleaned up. I was sewn up, and unhooked from some of the monitors.
I was supposed to move up to postpartum two hours after delivery, but I had a really hard time recovering from labor. I had lost a borderline scary amount of blood, and couldn't stand up in the time they needed me to. They ended up having to replace the catheter after my epidural was pulled (something I would NOT recommend right after pushing a watermelon out of your hoo-haw.) I cried and was shaking through the whole placement. I was pretty out of it still, and they started me on an iron drip to help with the dizziness and nausea.
6AM
I was still in labor and delivery, trying to recover when the nurse shift change came along. My new nurse was not my style, and I was grateful that I was feeling a little better because it meant I was moving out of her charge. I was able to get up, and walk to the bathroom, and then into the wheelchair so they could get me upstairs into a recovery room. We were so grateful to get up to postpartum, and we were finally able to get some quality sleep. Jack had his newborn tests, and slept like a champ in between. Nursing was established, and we were well on our way to getting home. We ended up staying one full day in postpartum, and it was honestly the best part of our entire stay. I was able to nap, shower, and snuggle my newborn--all while nurses brought me ice water and my meals.
Overall, I think this experience prepared me for parenthood by showing us just how unpredictable life with a child can be. When we started in on the induction process my expectation was that it would be 24 hours start to finish and I'd have a baby in my arms. Instead, I spent three days getting my body into labor, and then a full day in active labor before I was able to push and deliver the little guy. I am hopeful that I won't need to be induced for the next one, and that I can let my body do its thing. At my 6 week postpartum check, my regular midwife mentioned she was worried this wasn't a necessary induction. While I do see her thinking--I was 38 weeks with this little guy and he was already 9 pounds, 6 ounces. We both agreed that while it may not have been necessary, it probably saved me from pushing out a 10 or 11 pound baby, and for that I am grateful!